With an estimated 5 million Canadians suffering from irritable bowel syndrome (IBS), many people are looking for options to help relieve the symptoms associated with this condition. If you have been personally diagnosed with IBS, or have other gastrointestinal concerns, chances are you have heard about the low-FODMAP diet. First developed by Monash University in Melbourne, Australia, the low-FODMAP diet has been shown to alleviate the symptoms of IBS, such as flatulence, bloating, and altered bowel habits (constipation and/or diarrhea).
What are FODMAPs?
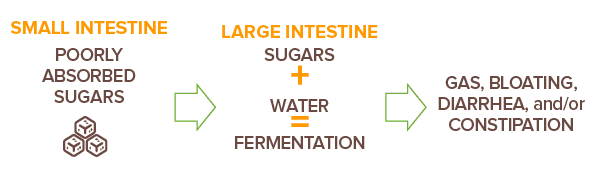
How can they affect your digestive health? FODMAP is an acronym for:
Fermentable, Oligosaccharides, Disaccharides, Monosaccharides, And Polyols
These are certain types of carbohydrates (sugars) found in our diet that are poorly absorbed in the small intestine in some individuals. Once these reach the large intestine, they bring water into the colon and are rapidly fermented creating symptoms such as gas and bloating. Examples of FODMAPs can include fructose found in apples, lactose found in dairy products, and polyols found in cauliflower. Although some individuals can absorb FODMAPs without any digestive concerns, those with IBS can experience bloating, gas, diarrhea, and/or constipation when consuming high-FODMAP foods.
The solution? A low-FODMAP diet.
In at least 10 randomized comparative trials, it has been shown that simply adjusting to a low-FODMAP diet can help about 50–80% of IBS patients achieve improvement in their condition.
The FODMAP diet consists of three steps.
- During the first step, individuals should avoid high-FODMAP foods by substituting these with low-FODMAP foods. For example, switch an apple for an orange, cauliflower for eggplant, and cow’s milk for almond milk! This phase lasts for 2–6 weeks and is best done with a health care practitioner who is educated about the FODMAP diet.
- Once this elimination phase is complete, individuals can move on to step two which involves reintroducing high-FODMAP foods and noting what symptoms they may trigger when consumed. Over 6–8 weeks, foods should be reintroduced one at a time and every few days, while still consuming foods that are low in FODMAPs.
- Establishing your own personal diet is the last step and it is in this phase where individuals consume the foods that are well tolerated and continue to avoid the foods that cause aggravating symptoms.
When we adjust our diets to include foods that have lower levels of FODMAPs, we make the job of our digestive tract easier and reduce the occurrence of unpleasant symptoms such as bloating, abdominal pain, constipation, and diarrhea. This is definitely a positive approach to managing IBS, however, what’s missing in a low-FODMAP diet? Better digestible fibre. Unfortunately, many high-fibre foods, and many fibre supplements, are high in FODMAPs, making it difficult for children and adults with IBS to meet the recommended daily intake of fibre in their diets. Keep in mind that soluble fibre is essential for gut health and regularity, and fibres such as inulin, bran, and wheat are high-FODMAP ingredients which are not beneficial for IBS and the digestive system.
PHGG has been shown to relieve constipation and gastrointestinal symptoms in people with IBS. Clinical studies show that IBS patients who consume 5–6 g of PHGG per day experience significantly reduced incidences of abdominal pain, gas, and bloating.2-4 Comparisons show that it is also much better tolerated than wheat bran for improving bowel habits. PHGG is also a low-FODMAP fibre and acts as a prebiotic. Of course, prebiotics are important for gut health due to their ability to support our gut bacteria. Research has also shown probiotics help support gastrointestinal health and reduce IBS-related complaints.5 Definitely a win for those with IBS and anyone who wants to support overall digestive health!

One helpful approach is to substitute these fibres with partially hydrolyzed guar gum (PHGG), a natural non-digestible dietary fibre made from the guar plant seed.
One helpful approach is to substitute these fibres with partially hydrolyzed guar gum (PHGG), a natural non-digestible dietary fibre made from the guar plant seed.

High- and Low-FODMAP Foods
| Food Category | High-FODMAP Foods | Low-FODMAP Foods |
| VEGETABLES | Artichoke, asparagus, cauliflower, garlic, green peas, leek, mushrooms, onion, sugar snap peas |
Aubergine/eggplant, beans (green), bok choy, capsicum (bell pepper), carrot, cucumber, lettuce, potato, tomato, zucchini |
| FRUITS | Apples, apple juice, cherries, dried fruit, mango, nectarines, peaches, pears, plums, watermelon | Cantaloupe, grapes, kiwi fruit (green), mandarin, orange, pineapple, strawberries |
| DAIRY AND ALTERNATIVES | Cow’s milk, custard, evaporated milk, ice cream, soy milk (made from whole soybeans), sweetened condensed milk, yogourt | Almond milk, brie/camembert cheese, feta cheese, hard cheeses, lactose-free milk, soy milk (made from soy protein) |
| PROTEIN SOURCES | Most legumes/pulses, some marinated meats/ poultry/seafood, some processed meats | Eggs, firm tofu, plain cooked meats/poultry/ seafood, tempeh |
| BREADS AND CEREAL PRODUCTS | Wheat/rye/barley-based breads, breakfast cereals, biscuits, and snack products | Corn flakes, oats, quinoa flakes, quinoa/rice/ corn pasta, rice cakes (plain), sourdough spelt bread, wheat/rye/barley-free breads |
| SUGARS/SWEETENERS AND CONFECTIONERY | High-fructose corn syrup, honey, sugar-free confectionery | Dark chocolate, maple syrup, rice malt syrup, table sugar |
| NUTS AND SEEDS | Cashews, pistachios | Macadamias, peanuts, pumpkin seeds, walnuts |
High- and Low-FODMAP Foods
| Food Category | High-FODMAP Foods | Low-FODMAP Foods |
| VEGETABLES | Artichoke, asparagus, cauliflower, garlic, green peas, leek, mushrooms, onion, sugar snap peas |
Aubergine/eggplant, beans (green), bok choy, capsicum (bell pepper), carrot, cucumber, lettuce, potato, tomato, zucchini |
| Food Category | High-FODMAP Foods | Low-FODMAP Foods |
| FRUITS | Apples, apple juice, cherries, dried fruit, mango, nectarines, peaches, pears, plums, watermelon | Cantaloupe, grapes, kiwi fruit (green), mandarin, orange, pineapple, strawberries |
| Food Category | High-FODMAP Foods | Low-FODMAP Foods |
| DAIRY AND ALTERNATIVES | Cow’s milk, custard, evaporated milk, ice cream, soy milk (made from whole soybeans), sweetened condensed milk, yogourt | Almond milk, brie/camembert cheese, feta cheese, hard cheeses, lactose-free milk, soy milk (made from soy protein) |
| Food Category | High-FODMAP Foods | Low-FODMAP Foods |
| BREADS AND CEREAL PRODUCTS | Wheat/rye/barley-based breads, breakfast cereals, biscuits, and snack products | Corn flakes, oats, quinoa flakes, quinoa/rice/ corn pasta, rice cakes (plain), sourdough spelt bread, wheat/rye/barley-free breads |
| Food Category | High-FODMAP Foods | Low-FODMAP Foods |
| PROTEIN SOURCES | Most legumes/pulses, some marinated meats/ poultry/seafood, some processed meats | Eggs, firm tofu, plain cooked meats/poultry/ seafood, tempeh |
| Food Category | High-FODMAP Foods | Low-FODMAP Foods |
| SUGARS/SWEETENERS AND CONFECTIONERY | High-fructose corn syrup, honey, sugar-free confectionery | Dark chocolate, maple syrup, rice malt syrup, table sugar |
| Food Category | High-FODMAP Foods | Low-FODMAP Foods |
| NUTS AND SEEDS | Cashews, pistachios | Macadamias, peanuts, pumpkin seeds, walnuts |
References
- Staudacher HM & Whelan K. The low-FODMAP diet: recent advances in understanding its mechanisms and efficacy in irritable bowel syndrome. Gut. 2017; 66:1517-1527.
- Niv E, Halak A, Tiommny E, et al. Randomized clinical study: Partially hydrolyzed guar gum (PHGG) versus placebo in the treatment of patients with irritable bowel syndrome. Nutr Metab (Lond.). 2016; 13:10.
- Parisi GC, Zilli M, Miani MP, et al. High-fiber diet supplementation in patients with irritable bowel syndrome (IBS). Comparison between wheat bran diet and partially hydrolyzed guar gum (PHGG). Dig Dis Sci. 2002; 47(8):1697-1704.
- Kapoor M, Sugita M, Fukuzawa Y, et al. Impact of partially hydrolyzed guar gum (PHGG) on constipation prevention: A systematic review and meta-analysis. J Func Foods. 2017; 33:52-66.
- Didari T, Mozaffari S, Nikfar S, et al. Effectiveness of probiotics in irritable bowel syndrome: Updated systematic review with meta-analysis. World J Gastrolenterol. 2015; 21(10):3072-84.