THE GUT-STRESS LINK
I think we are all aware of the fact that long-term exposure to stress is a contributing factor to the development of numerous diseases. Much has been written about this association and even more published in peer-reviewed journals. The conclusion is that stress can seriously impact overall well-being leading to numerous health consequences.
However, the relationship between stress and illness is complicated and one’s susceptibility to stress depends on numerous factors. For example, the ability of individuals to cope with stress, their personality traits, and their genetic predisposition can all have impact. We know that chronic stress has a significant effect on the immune system eventually leading to a multitude of complications. For example, studies show that it can raise catecholamine and suppressor T cells levels, ultimately suppressing the immune system leading to viral infections that include the common cold and influenza just to name a few.
We also know that stress can have an impact on acid concentration in the stomach, contribute to the buildup of plaque in the artery walls leading to heart disease, and can be a factor in Crohn’s disease, ulcerative colitis, and even the development of cancer all by impacting natural killer cells’ activity. We also know that increases in stress levels can worsen the symptoms associated with fibromyalgia and central sensitization syndrome (CSS) conditions – how does that happen?
OUR STARTING POINT
In order to understand how chronic stress can impact so many symptoms we really need to have a quick review of the gastrointestinal tract (we’ll call it the “gut” for simplicity). As most of you know, the “gut” has received much press in the last decade for numerous reasons, led by a high level of interest in probiotics. We have learned about the incredible “microbiome”, defined as the collection of microbes or micro-organisms inhabiting the gut and creating a kind of mini-ecosystem. Scientists are now spewing out thousands of published papers every year on the association between the microbiome and health. In turn this is beginning to create a new understanding of how important the gut is to overall general health. 
Interestingly, what scientists are now figuring out, Hippocrates – known as the father of medicine – had already figured out over 3,000 years ago, when he accurately stated that, “health begins in the gut.” In Integrative Medicine we often say that, “the caveat of all healing is the gut.” This has deep meaning, because it is really saying that we can’t really achieve optimal health unless the gut is itself healthy. My nearly 25 years of clinical practice definitely support this premise and has allowed me the privilege of improving the health of thousands of people.
THE GUT FACTS
Today we know that the gut is not only a place of digestion where nutrients are absorbed and wastes eliminated, but also a place where other critically important functions occur. These are functions we wouldn’t necessarily associate with the gut, yet they are, and they are functions vitally important to the health of the human body.
Nearly 80% of our immune system is located in the gut
This is an amazing fact and when you start reviewing the reasons, two main points stand out. First, the most abundant immunoglobulin making up 80% of all the antibodies in our system is known as IgG, and 100% of all IgG is made in the gut. Based on this fact alone, we can say that 80% of our immune system comes from the gut. Secondly, if you think about which part of the human body has the most exposure to the external environment, it is, hands down, the gut. The gastrointestinal tract has about 430 sq. ft. of surface area, so more material comes into contact here than any other place in our body. Therefore, if you were to protect your house from burglars, where would you put the guards? You would place them in the main entry points, the front and back doors! In the body, the intelligent immune system would do the same, it places its guards in the main entry point, the gut. So damage to the gut, would also have impact on overall immune function.
There are as many neurotransmitters produced in the gut as there are in the brain
This is an interesting, yet underappreciated revelation especially when it comes to stress and anxiety. Research has shown that one of the most important neurotransmitters, the feel-good hormone, serotonin, is also produced in the gut. In fact, between 80–95% of all serotonin comes from the gut! This is an incredible revelation since we are continually trying to increase the levels of this hormone using numerous types of anti-depressant drugs. Could improving gut function, also improve serotonin production, thus helping us feel better about ourselves and helping us sleep? As we noted earlier in Part 1 of the article fibromyalgia, patients have reduced levels of serotonin probably contributing to the ongoing sleep issues.
There over 100 trillion bacteria in your gut
Imagine the magnitude of this number and think what these little microorganisms are doing in your gut. Much research is being done on these little critters and what we are learning is nothing short of amazing. They are vital to maintaining immune function, the integrity of the gut lining, controlling pathogenic bacteria from proliferating, and even keeping our brains in functional order. Recent research into fecal transplantation is giving us new insights and opening up new avenues of treatment that could become the norm in the future. As an example, I want to share a case that gives us incredible insights into the power of gut bacteria. A 38-year old contracted C. difficile (one of the most dreaded gastrointestinal infections). She had chronic diarrhea and is placed on IV antibiotics. For three months she was hospitalized with no resolution to her infection. She lost nearly 40 lbs and was in critical condition. 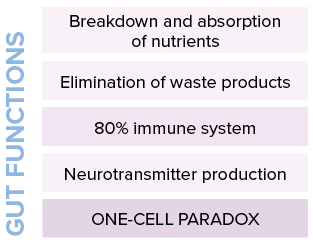 The GI specialist went into her husband’s gut and isolated bacteria that he then transplanted into the patient. Within three days the C. difficile was completely eradicated and the patient was back to normal. Incredible! What the most powerful antibiotics in the world couldn’t kill in three months, healthy bacteria (from the gut of a healthy human) got rid of in less than three days. This type of treatment has been implemented over 1,000 times with the same outcome. And stories like these merely scratch the surface when it comes to the importance of a healthy gut and the bacteria it contains.
The GI specialist went into her husband’s gut and isolated bacteria that he then transplanted into the patient. Within three days the C. difficile was completely eradicated and the patient was back to normal. Incredible! What the most powerful antibiotics in the world couldn’t kill in three months, healthy bacteria (from the gut of a healthy human) got rid of in less than three days. This type of treatment has been implemented over 1,000 times with the same outcome. And stories like these merely scratch the surface when it comes to the importance of a healthy gut and the bacteria it contains.
THE ONE-CELL PARADOX
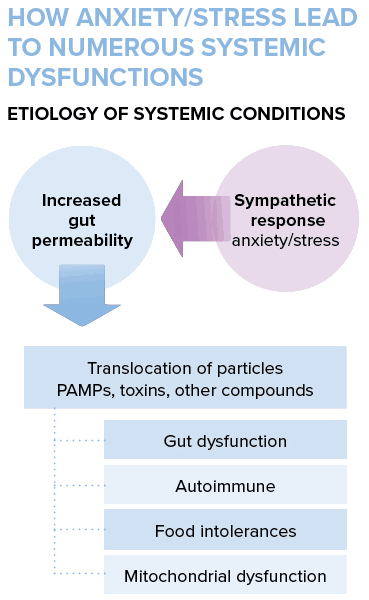
The one-cell paradox refers to the fact that what separates everything in the gut from entering the bloodstream is actually one cell. In other words, a microscopic entity is all that stands in the way of bacteria, bacterial cell particles known as PAMPs (pathogen associated molecular patterns), toxins, and other compounds from entering the blood- stream. We call this a paradox because not only does this one cell lining need to be strong enough to block these compounds from entering the blood, but at the same time it needs to be permeable enough to allow nutrients to get into the blood. So it is indeed a paradox. It is this “one-cell paradox” that’s at the fulcrum of many health conditions and most impacted negatively by stress. The breakdown of this lining, known as “increased gut permeability” can create an enormous amount of problems systemically throughout the body.
STRESS + GUT = SYMPTOMS
Now that we have a better understanding of the function of the gut we can begin to look at the influence that stress and the gut may have on the symptoms of fibromyalgia. Look more closely at the one-cell layer (epithelial layer) that separates everything in the gut from the blood, and we find an intricate array of proteins known as “tight junctions” firmly holding these epithelial cells together. The movement of nutrients and other materials through this thin wall is closely monitored and controlled to ensure proper translocation. When this system is functioning properly, we’re good to go, as they say. However, there are numerous events that can occur to cause dysfunctionality and eventually break down in this carefully controlled “gating system.” How many of us have experienced some form of digestive problem? Everyone! Who hasn’t had an upset stomach, gas, bloating, diarrhea, or even a bout of constipation? We have all gone through this, but few have ever considered the consequential effects of chronic gut issues. Even fewer have associated poor gut function with health problems like fibromyalgia or heart disease, eczema, arthritis, chronic fatigue, autoimmune disorders, and so on. And how many would associate the chronic use of antacids with food allergies and autoimmune diseases. Although all the aforementioned are all important consequential outcomes of poor gut function, none is more important than the contribution of stress. When we are stressed the brain triggers something known as the sympathetic response to protect itself, and this is when the gut’s epithelial lining (the one cell separation) can become compromised. This is the result of the flight or fight response, where the sympathetic response takes blood from the gut (core) and moves it to the peripheral tissues (limbs) to allow the zebra to run away from the lion. In the human body, when we have ongoing stress and anxiety for long periods of time, the sympathetic response is continually turned on, creating long-term “increased gut permeability”, and thus long periods of translocation of PAMPs and other compounds. The result of this translocation can be autoimmune disease, food intolerances, mitochondrial dysfunction (leading to fatigue, sleep issues, cognitive issues, etc.) and systemic inflammation.
A SIMPLIFIED LOOK
To visualize “increased gut permeability” and its impact on health is to visualize a roof on your house. The roof on your house is your gut lining (one cell thick) and inside your house are things analogous to parts of your body. The sofa for example is your skin; the hinges on the doors are your joints; the furnace is your lungs; and the television is your brain; and so on. Now imagine if you had holes in your roof during the “rainy season”. Water would fall on different items around the house. If it drips on the television/brain, it could lead to cognitive dysfunction or brain fog. If it fell on the door hinges/joints they would rust, leading to painful joints. And if the water landed on the furnace/lungs, the result could be asthma. This is how a “leaky gut” similar to a “leaky roof” can inflict all sorts of dysfunctions on the human body – our house. Now we can understand why all patients with fibromyalgia have increases in their symptoms when they experience levels of stress. The translocation of compounds like PAMPs can impact mitochondria influencing energy production. Therefore, it stands to reason, that in CSS or fibromyalgia, stress/anxiety must be looked at as a key-contributing factor and therefore foundational in any treatment plan.