Nearly two decades ago this kind and compassionate gentleman was representing a client who had been diagnosed with FM and was attempting to get disability compensation. He informed me that even with all the information available to him at the time, the judge threw the case out of court, saying that FM really didn’t exist and that it was all in his client’s head.
The story angered me and gave me perspective on the challenges and difficulties women encounter with this stressful condition. Having a deeper understanding, elevated my motivation to even greater heights in trying to make the lives of these sufferers better. FM was not very well understood, not very well accepted, and definitely not well treated. This story made me think how far we’ve come along and where we need to go to improve life for those who endure this difficult- to-treat condition.
WHAT IS FIBROMYALGIA?
Fibromyalgia can be classified as a complex chronic disease, causing pain, tenderness and stiffness in muscles, joints, and tendons. In almost all cases, the FM patient also report debilitating fatigue, post-exertion malaise, sleep difficulties, cognitive dysfunction in the form of brain fog and memory problems, and gastrointestinal issues often presenting as irritable bowel syndrome (IBS).
Interestingly, there are a number of other complex chronic diseases that share many of the symptoms of FM and thus fall in the same classification. These include myalgic encephalo-myelitis, chronic fatigue syndrome, chronic Lyme disease, and multiple chemical sensitivities. These conditions carry many
of the same symptoms with the exception of the pain that is always found in FM.
The important aspect here are the symptoms – which possibly point to the same dysfunction underlying in all these afflictions. As we’ll learn, although there are numerous possible physiological dysfunctions, most would agree that energy production is at the fulcrum of the disorder.
HOW IS FIBROMYALGIA
DIAGNOSED?
The problem with FM is that many of its main symptoms are found in other health conditions. For example, hypothyroidism (thyroid gland not making enough hormones), rheumatoid arthritis, lupus, osteoarthritis, ankylosing spondylitis (inflammation of the spine), and polymyalgia rheumatica all cause pain, muscle aches and fatigue, similar to FM. So a key aspect of the FM diagnosis is to rule out these and other possible conditions with similar symptom patterns to FM.
Part of the difficulty in diagnosing FM is that there are no blood tests or objective measureable parameters to help the physician in confirming the diagnosis. The majority of the testing done is to exclude other possible diagnoses.
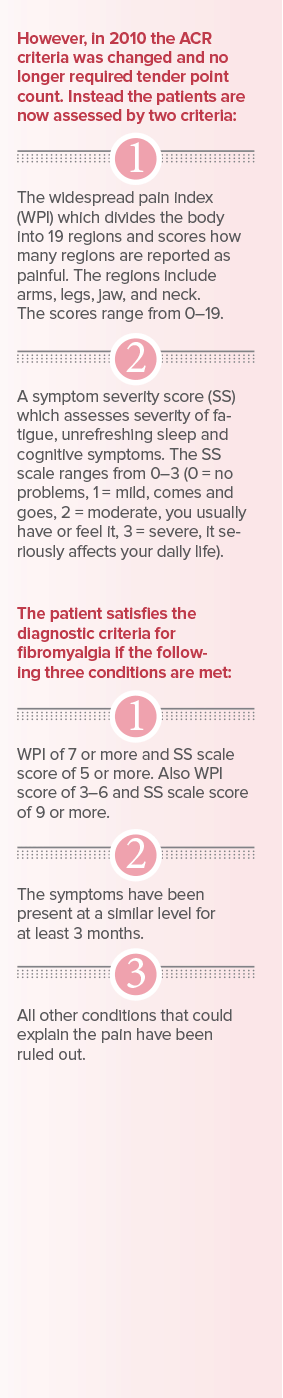
As we continue to pursue research and better understand FM so will our diagnostic testing. Interestingly over the last two decades many physicians have used the American College of Rheumatology (ACR) criteria. The 1990 ACR criteria for FM involved testing tender points in various locations of the body; if 11 of the 18 connective tissue areas were tender when pressure was applied, and no other explanation for the pain was found, then the person was likely to have fibromyalgia.

GENDER SPECIFICS
There is little argument that FM is more prevalent in women than men. Statistics show that up to 90% of all people with FM are women and my clinical experience absolutely support this theory. Although the exact reasons behind this gender difference is not known, hormones and possibly women’s stress levels may be a contributing factor.
Interestingly, besides the common symptoms of FM (fatigue, post-exertion malaise, pain, cognitive dysfunction, sleep issues, possible IBS), women may also experience: migraines, painful periods, irritable bladder, restless leg syndrome, and hypersensitivities.
FIBROMYALGIA CAUSES
Although the exact cause of FM remains unknown, there are numerous theories and also some signs that give insights into probable origins. From all reports it appears that FM results from a combination of physical and emotional stressors; in other words it is multifactorial. In many cases we find that the onset of FM is associated with an infection, a trauma (motor vehicle accident) or a psychological stress. There are
also numerous compounds out of sync that give us insights into what may be happening. For example, serotonin, the well-known feel-good hormone (the one that helps you sleep and reduces the feelings of anxiety) is low in the brains of FM patients. These patients also have elevated levels of a chemical called substance P, which increases pain signals.
Neurophysiological changes are definitely present in fibromyalgia and in a certain sense they confirm that an underlying pathophysiology is present. For example, abnormalities in pain processing mechanism create a myriad of symptoms that include myalgia (muscle pain), arthralgia (joint pain), and neuralgia (nerve pain). All this has led to grouping FM with other complex diseases under the central sensitivity syndrome family (CSS). CSS is defined as a state where the central nervous system amplifies sensory input across many systems. In simple terms this means that what might normally be perceived as slight pain gets amplified to intense pain (hyperalgesia) and what may never cause pain such as “a light touch” becomes interpreted as pain (allodynia). In the end, these various
dysfunctions create the rather confusing symptomology of fibromyalgia pain.
MITOCHONDRIAL LINK
When you look at the symptoms associated with many of the CSS conditions including fibromyalgia, the cells mitochondria are at the centre of the discussion. To better understand what they do and how they work I am going to tell you a story.
When you think about the most important element in life, it is not food and water, because we can go without food and water for days, even weeks, but what we can’t go without for not even for two minutes is air. The critical component in air, the key to sustaining life, is oxygen. If we are deprived of oxygen for even a few minutes, the consequences are serious, even fatal. So what is oxygen doing that makes it so critically important?
Oxygen is carried to every cell of the body by red blood cells. Once it enters a muscle cell where fibromyalgia patients feel their pain and fatigue, or a brain cell where they feel their cognitive dysfunction what happens?
When oxygen enters a cell it is solely utilized by the mitochondria. Each cell contain over 1,500 of these energy producing organelles, and they create the electricity (energy) that allows us to function.
The mitochondria are like hydro dams, and oxygen flows through them like water. Just as water falls down the dam, turning the turbines and producing the electricity that lights up our cities, in the body the oxygen flowing through the mitochondria produces the electricity that “lights up” our lives. Every single function in the body is reliant on
this energy production cycle. Imagine if we didn’t have it, we wouldn’t be able to function. It would be like taking cyanide. Do you know how this deadly poison works? It simply stops oxygen’s ability to flow through the mitochondria. There is very strong evidence that many CSS diagnoses, including FM are mitochondrial dysfunctions. And when one looks at the key symptoms of CSS patients, they are all tied to energy production issues.
So the next important question is how do the mitochondria become
dysfunctional? There are numerous possibilities here – viral and bacterial infections, PAMPS (pathogen-associated molecular patterns) bacterial cell walls entering the blood from the gut interfering with mitochondrial energy production, nutritional deficiencies, and stress. To better understand some of these possibilities a closer look at the gut and stress is a good starting point.
Please look for the next Women’s Voice issue for Part 2 of this article.